Advances in Amyloid Research: Formation, Detection, Therapy
This article looks at amyloid proteins, including their genesis, structural properties, and associated disorders. It also looks at detection methods and therapeutic tactics, emphasizing recent advances and challenges in the field.
Introduction to Amyloids
Amyloids are protein assemblages with a fibrous shape and cross-β structure, as described by Chatani and Yamamoto (2017). These structures are generated through the process of molecular recognition and self-assembly, in which a peptide or protein monomer spontaneously self-associates into dimers and oligomers, then into supramolecular aggregates, and lastly condensed fibrils (Hauser et al., 2014). Amyloid fibrils have a high degree of -sheet in a traditional ”cross-” pattern, a fibrillar shape in electron microscopy, and the capacity to bind and modify the spectroscopic characteristics of heteroaromatic dyes Congo red and thioflavin T (O’Nuallain & Wetzel, 2002). Amyloid -peptide (A) accumulates in the brain in all types of Alzheimer’s disease (AD) (Eckman et al., 2006). Amyloid deposits in Alzheimer’s disease include insoluble plaques, intracellular Aβ, and soluble oligomers. The link between these deposits and their clinical importance is unknown (Kayed et al., 2007).
Amyloid fibrils are linked to a variety of disorders, including Alzheimer’s and type 2 diabetes. Alzheimer’s disease is characterized by the deposition of amyloid -peptide (A) in the brain (Eckman et al., 2006). The hazardous form of amyloidogenic proteins, known as membrane-permeant oligomers, has been linked to proteotoxicity in β cells in type 2 diabetes (Gurlo et al., 2010). As a result, amyloid fibrils and their precursor oligomers play an important role in the development of these disorders.
Formation and Characteristics
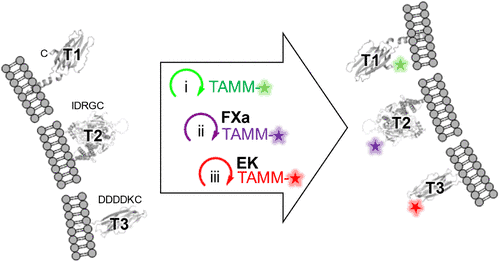
Amyloid fibril formation is a nucleation-dependent polymerization process that involves the assembly of non-native precursor proteins into nuclei, which then grow via an extension reaction involving the sequential incorporation of proteins. This results in the formation of rigid and straight morphology consisting of several layers of cross-β sheets (Makin et al., 2005; Xue et al., 2016; Frankó et al., 2018). This process is similar to crystallization, including supersaturation-dependent nucleation and growth phases (Zhu et al., 2002; Bieschke et al., 2010). The creation of amyloid fibrils is a universal mechanism that involves delayed nucleation followed by exponential growth of amyloid particles. Secondary events such as fibril fragmentation and aggregate surface-catalyzed heterogeneous nucleation speed up the process. The dynamics of amyloid fibril production are characteristic of a nucleation-dependent polymerization mechanism, with initial amyloid fibril creation occurring intracellularly, followed by membrane rupture and further seeding activities that result in extracellular amyloid deposits.
Amyloids have a distinct cross-β structure with aromatic rings stacked and polypeptide β-strands running perpendicular to the fibril axis (Zhu et al., 2002). Furthermore, amyloid fibrils are resistant to proteolysis and have a stable formation, which is important for understanding their role in disorders such as Alzheimer’s and Parkinson’s (Makin et al., 2005; Frankó et al., 2018; Bieschke et al., 2010).
Amyloid fibril formation is a complex process requiring nucleation-dependent polymerization, and amyloids’ physical features, such as their distinct shape and resistance to proteolysis, contribute to their importance in a variety of biological processes and disorders.
Detection and Therapeutic Approaches
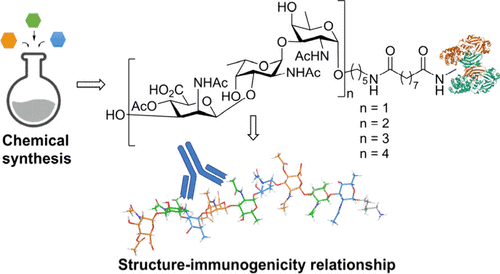
The detection of amyloid deposits in tissues is critical for the diagnosis and treatment of amyloid-related diseases. Congo red staining is the gold standard for detecting amyloid deposits in tissues (Rahman et al., 2021). Recent advancements, such as molecular scintigraphy imaging, allow for non-invasive detection of amyloid deposits in the myocardium, reshaping clinical practice and eliminating the need for endomyocardial biopsy (Simões, 2021). PET imaging has improved the detection of β-amyloid accumulation in vivo, transforming Alzheimer’s disease into a dynamic clinicobiological entity (Leuzy et al., 2014). Furthermore, a unique method for detecting amyloid deposits in human tissues employing a fluorescent dye has been created, indicating that it is a new and promising approach.
Therapeutic therapies for amyloid-related illnesses are designed to prevent amyloid production and improve clearance. Several therapeutic approaches have been proposed, including the use of inhibitors to prevent amyloid-β fibril formation (Lashuel et al., 2002), agents to interfere with fibril growth (Madine et al., 2008), and the use of neprilysin to reduce brain amyloid burden as a novel approach for treating Alzheimer’s disease (Guan et al., 2008). Furthermore, the development of amyloid imaging agents for PET has garnered considerable interest as a powerful tool for measuring amyloid biomarkers (Furumoto et al., 2007). Metal chelation therapy and Aβ vaccination have been proposed as potential clinical treatments (Rosenberg, 2003). Furthermore, inhibiting amyloid formation, disrupting produced amyloids, and lowering amyloid-induced oxidative stress are possible therapeutic options for amyloid-related degenerative illnesses (Amini et al. 2014).
To summarize, recent advances in amyloid detection technologies, like as molecular scintigraphy and PET imaging, have transformed the diagnosis and understanding of amyloid-related illnesses. Therapeutic options, including as the creation of inhibitors, amyloid imaging agents, and vaccination methods, show promise for avoiding amyloid production and boosting clearance in a variety of amyloid-related illnesses.
References
Chatani, E. and Yamamoto, N. (2017). Recent progress on understanding the mechanisms of amyloid nucleation. Biophysical Reviews, 10(2), 527-534. https://doi.org/10.1007/s12551-017-0353-8
Eckman, E., Adams, S., Troendle, F., Stodola, B., Kahn, M., Fauq, A., … & Eckman, C. (2006). Regulation of steady-state β-amyloid levels in the brain by neprilysin and endothelin-converting enzyme but not angiotensin-converting enzyme. Journal of Biological Chemistry, 281(41), 30471-30478. https://doi.org/10.1074/jbc.m605827200
Gurlo, T., Ryazantsev, S., Huang, C., Yeh, M., Reber, H., Hines, O., … & Butler, P. (2010). Evidence for proteotoxicity in β cells in type 2 diabetes. American Journal of Pathology, 176(2), 861-869. https://doi.org/10.2353/ajpath.2010.090532
Hauser, C., Maurer‐Stroh, S., & Martins, I. (2014). Amyloid-based nanosensors and nanodevices. Chemical Society Reviews, 43(15), 5326. https://doi.org/10.1039/c4cs00082j
Kayed, R., Head, E., Sarsoza, F., Saing, T., Cotman, C., Necula, M., … & Glabe, C. (2007). Fibril specific, conformation dependent antibodies recognize a generic epitope common to amyloid fibrils and fibrillar oligomers that is absent in prefibrillar oligomers. Molecular Neurodegeneration, 2(1). https://doi.org/10.1186/1750-1326-2-18
O’Nuallain, B. and Wetzel, R. (2002). Conformational abs recognizing a generic amyloid fibril epitope. Proceedings of the National Academy of Sciences, 99(3), 1485-1490. https://doi.org/10.1073/pnas.022662599
Bieschke, J., Russ, J., Friedrich, R., Ehrnhoefer, D., Wobst, H., Neugebauer, K., … & Wanker, E. (2010). Egcg remodels mature α-synuclein and amyloid-β fibrils and reduces cellular toxicity. Proceedings of the National Academy of Sciences, 107(17), 7710-7715. https://doi.org/10.1073/pnas.0910723107
Frankó, A., Camargo, D., Böddrich, A., Garg, D., Camargo, A., Rathkolb, B., … & Angelis, M. (2018). Epigallocatechin gallate (egcg) reduces the intensity of pancreatic amyloid fibrils in human islet amyloid polypeptide (hiapp) transgenic mice. Scientific Reports, 8(1). https://doi.org/10.1038/s41598-017-18807-8
Makin, O., Atkins, E., Sikorski, P., Johansson, J., & Serpell, L. (2005). Molecular basis for amyloid fibril formation and stability. Proceedings of the National Academy of Sciences, 102(2), 315-320. https://doi.org/10.1073/pnas.0406847102
Xue, W., Pierpoint, R., & Doumic, M. (2016). Insights into the variability of nucleated amyloid polymerization by a minimalistic model of stochastic protein assembly. The Journal of Chemical Physics, 144(17). https://doi.org/10.1063/1.4947472
Zhu, M., Souillac, P., Ionescu-Zanetti, C., Carter, S., & Fink, A. (2002). Surface-catalyzed amyloid fibril formation. Journal of Biological Chemistry, 277(52), 50914-50922. https://doi.org/10.1074/jbc.m207225200
Amini, R., Yazdanparast, R., & Ghaffari, S. (2014). Apigenin modulates the expression levels of pro-inflammatory mediators to reduce the human insulin amyloid-induced oxidant damages in sk-n-mc cells. Human & Experimental Toxicology, 34(6), 642-653. https://doi.org/10.1177/0960327114554046
Furumoto, S., Okamura, N., Iwata, R., Yanai, K., Arai, H., & Kudo, Y. (2007). Recent advances in the development of amyloid imaging agents. Current Topics in Medicinal Chemistry, 7(18), 1773-1789. https://doi.org/10.2174/156802607782507402
Guan, H., Liu, Y., Daily, A., Kim, M., Oddo, S., LaFerla, F., … & Hersh, L. (2008). Peripherally expressed neprilysin reduces brain amyloid burden: a novel approach for treating alzheimer’s disease. Journal of Neuroscience Research, 87(6), 1462-1473. https://doi.org/10.1002/jnr.21944
Gusel’nikova, V., Antimonova, O., Fedorova, E., Shavlovsky, M., Safray, A., Rukavishnikova, A., … & Korzhevskii, D. (2020). A novel method for amyloid detection in human tissue load using a fluorescent dye — congo red analogue. Sovremennye Tehnologii v Medicine, 12(1), 65. https://doi.org/10.17691/stm2020.12.1.08
Lashuel, H., Hartley, D., Balakhaneh, D., Aggarwal, A., Teichberg, S., & Callaway, D. (2002). New class of inhibitors of amyloid-β fibril formation. Journal of Biological Chemistry, 277(45), 42881-42890. https://doi.org/10.1074/jbc.m206593200
Leuzy, A., Zimmer, E., Gauthier, S., & Rosa-Neto, P. (2014). Amyloid imaging in alzheimer’s disease: a potential new era of personalized medicine?. Translational Neuroscience, 5(1). https://doi.org/10.2478/s13380-014-0205-y
Madine, J., Doig, A., & Middleton, D. (2008). Design of an n-methylated peptide inhibitor of α-synuclein aggregation guided by solid-state nmr. Journal of the American Chemical Society, 130(25), 7873-7881. https://doi.org/10.1021/ja075356q
Rahman, M., Schmuck, B., Hansson, H., Härd, T., Westermark, G., & Sandgren, M. (2021). Enhanced detection of attr amyloid using a nanofibril-based assay. Amyloid, 28(3), 158-167. https://doi.org/10.1080/13506129.2021.1886072
Rosenberg, R. (2003). Metal chelation therapy for alzheimer disease. Archives of Neurology, 60(12), 1678. https://doi.org/10.1001/archneur.60.12.1678
Simões, M. (2021). Cardiac scintigraphy with bone markers in clinical practice: when to solicit the exam? how to interpret the results?. Abc Heart Failure & Cardiomyopathy, 1(2), 127-129. https://doi.org/10.36660/abchf.20210022